MYOPIA, RETINAL BREAKS, RETINAL DETACHMENT
EYE - A CAMERA
Our eyes are living cameras. Eye has a film in the form of retina. It also has focusing system in the form of cornea and lens which make the light rays to focus on the retina.
The following figure shows the similarity between eyeball and camera:
NORMAL VISION
The light emerging from the objects we see, is made to focus on retina by eye’s focusing system (cornea and lens). Thus an image is formed on retina which is transferred to brain by optic nerve, where the photo is printed and vision is perceived.
REFRACTIVE ERRORS-
Myopia, Hypermetropia,Astigmatism
If the light is focused on the retina, we get a normal crisp vision. If in case, the light is focused ‘in front’ or ‘behind’ the retina, we get a defocused blurred image. These conditions are called refractive errors. In these conditions, we try to bring the focus back on retina by glasses or contact lenses.
Myopia
If the light rays are focusing ‘in front’ of retina, its called myopia (Near sightedness). These people can see near objects clearly but far objects are blurred. People with myopia are called as “Myopes”. Myopia can be corrected by Minus glasses.
Hypermetropia
The light focuses behind the retina. They have good far vision. ( Thus called Far Sightedness). This can be corrected by Plus glasses.
Astigmatism
In this condition the focusing of light varies in different meridians. These people have distorted vision. Objects may appear to tilt. This is corrected by Cylindrical glasses.
MYOPIA -RETINAL BREAKS &
RETINAL DETACHMENT
Our eye has a film in the back of it, just like a camera film. This living film is called as Retina. Unlike the camera film, retina is attached like a sticker to the wall of eyeball. If by any chance it gets detached , it stops working, leading to blindness.
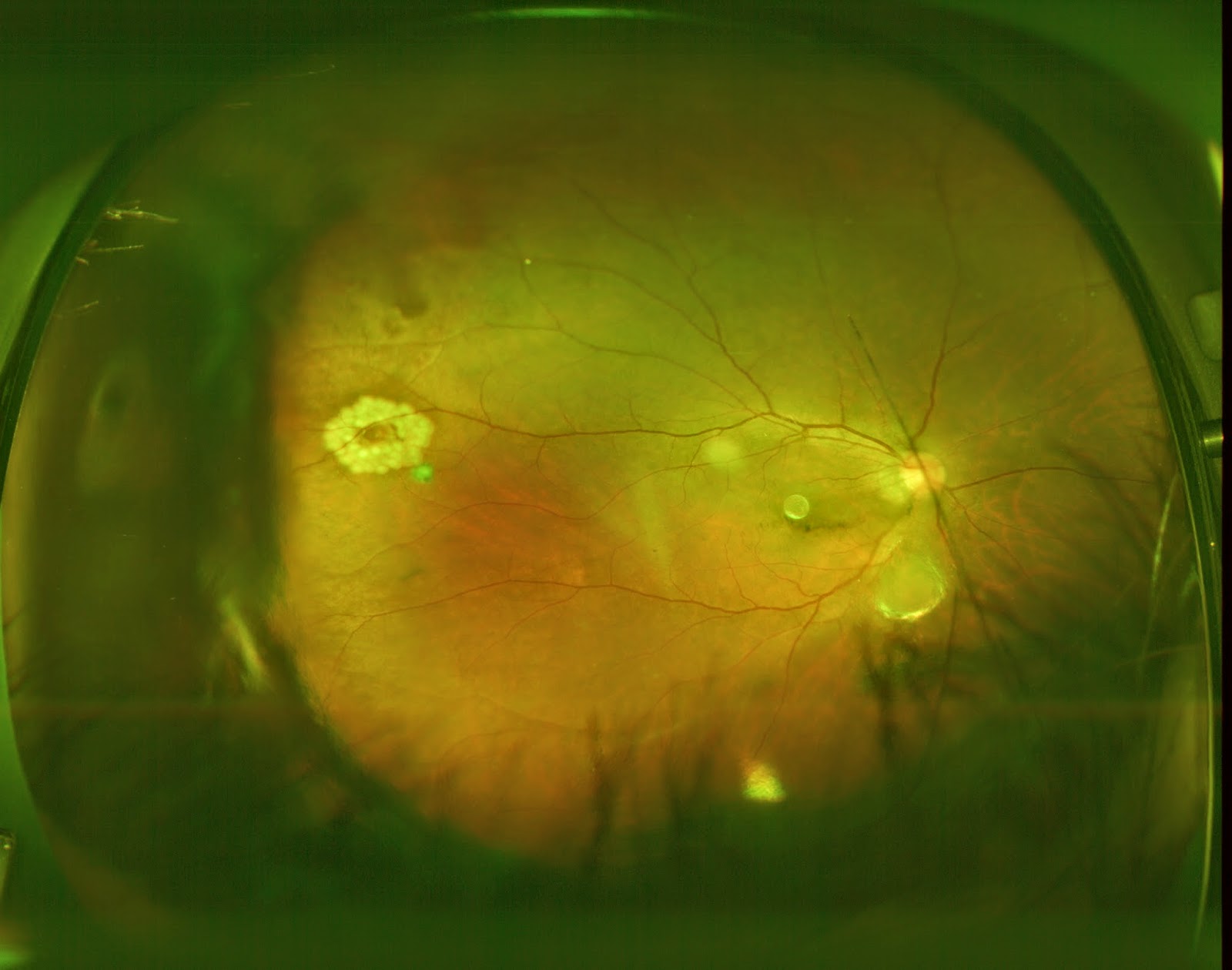
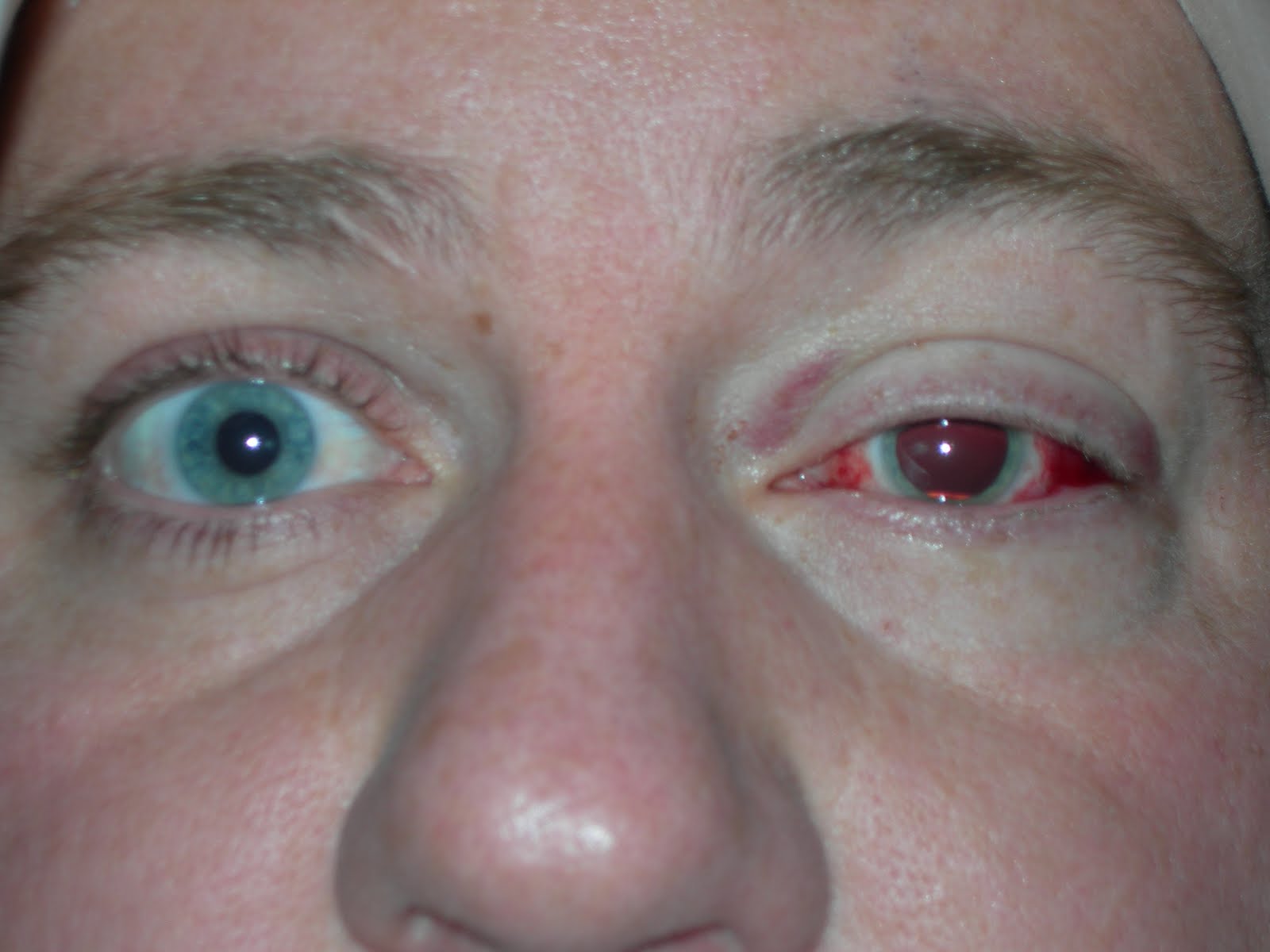
Normal retina is like a thin plastic sheet. This is spread over the inner surface of eye ball like a sticker. Eye ball is filled with vitreous gel which helps in attaching the retina to the surface. In myopia the eye ball is big. The inner surface area is more than normal. To cover this extra inner surface , the retina gets stretched. So the retina in myopes is much thinner and stretched. As the time goes, this thin retina can become friable in certain areas which are called as Retinal degenerations. Later they may tear up causing “Retinal Holes” or “Retinal Breaks”. If untreated at this stage , these holes can become access points to water in vitreous gel. Once the water enters these breaks, it reaches beneath the attached sticker (Subretinal Space). From here it spreads beneath the retina and detaches it from its surface. This is called as Retinal Detachment (RD). The detached retina loses its food supply and starts dying within hours. Patient loses vision and may become blind for the rest of his life. RD is a serious blinding eye disorder. RD can lead to permanent blindness. This condition can be prevented by timely treatment of retinal breaks.


MYOPIA AND RETINAL DETACHMENT-
FEW QUESTIONS -THEIR ANSWERS:
1. What are retinal degenerations and retinal breaks? Why are myopes at more risk of developing them?
In myopia, the retina is stretched out and thus is thinner than normal. Such thin retina becomes eroded in certain areas . These weakened areas are called retinal degenerations. These may later break causing a hole in the retina. These are called as retinal breaks or holes.
Consider a thin cloth. You stretch it with both hands. As you stretch it further, it becomes thinner in certain areas and later gets torn. Retina in Myopes behaves in similar way.
2. How do I know if I have retinal breaks?
There is no way that you will know of their presence. There are no symptoms nor indications. Only a retinal surgeon can detect these holes. Occasionally few patients can have floaters or flashes of light when they develop breaks. You should not rely on these symptoms as they are seen in only small percentage of retinal holes.
3. Can the retinal holes be prevented?
Absolutely no. The thin retinal nature comes by birth. It cannot be modified. So the holes cannot be prevented. Can u make a dwarf become tall? No. Certain things cannot be prevented or changed. Retinal breaks are one of those.
4. What are the complications of retinal breaks?
Retinal breaks if not treated early, can lead to Retinal Detachment and blindness.
5. What is Retinal Detachment?
Normally the retina is attached like a sticker to the underlying layer. The separation of retina from the inner surface of eye is called as RD. RD is a serious blinding disorder.
6. Can Retinal Detachment be prevented?
Certainly yes. It can be prevented by regular retinal screening examination and timely laser barrage to retinal holes.
7. What is retinal screening and prevention?
Patients with retinal holes do not have any eye problem or symptoms. It is the retinal surgeon, who after examination, detects these holes. The examination which he does to detect these holes is called as Retinal Screening. In case of a hole being detected, he does a laser treatment to seal off the holes . This treatment done to prevent RD is called “Prophylaxis” (Preventive treatment ).
Retinal Holes are like bombs being hidden in your eyes. All myopes are at risk to have these bombs. If not disconnected and removed at right time, the bomb may explode and cause serious damage. Similarly retinal hole if not treated , can explode in the form of RD and cause serious blindness. The test done by Retinal surgeon to detect these bombs is called as Retinal Screening. The laser treatment which he does to disconnect these bombs is called as “Prophylactic LASER barrage” .
8. Who should undergo retinal screening?
Any myope with more than -3 Diopter glass power should undergo yearly retinal screening.
9. How often should retinal screening be done?
Usually you should get it done every year, Unless your retinal surgeon advices otherwise.
10. I am a myope with -5 D glass power. I don’t have any problem with my eyes. I have absolutely no symptoms. Should I still undergo retinal examination?
Absolutely yes. By the time you develop symptoms, you may already have developed RD. Then you may become blind for the rest of your life.
11. What is Pupil dilatation?
Retina is inside the eye ball. Its like a movie screen inside the theater. The only way to look at it is a small window in our eye, which is called pupil. It is like peeping through the window to watch the movie. The more the window is open , the more the view of screen. Normally the pupil is small, allowing us only partial view of retina. Pupil should be widened to give the full view of retina. The process by which pupil is dilated is called as pharmacodilatation. This is done by instilling eye drops. It takes 30 min. to one hour for full dilatation. After the dilatation, persons near vision will get blurred for few hours. Also he has Photophobia (Inability to see light) for few hours. All these are temporary.
12. What is “Prophylactic Laser Barrage”?It s a treatment done for the retinal Breaks or degenerations, to prevent Retinal Detachment. It aims at creating a Barrage (Fence/Dam) around the dangerous lesions (The danger areas). LASER is passed onto the retina and it is welded around the lesions. This adhesive fence which is created , blocks the water to spread beneath the retina. Thus it prevents RD.
It is a minor procedure done in doctor’s room. It is done under topical anesthesia (eye drops). It needs less than 10 minutes. No injection or rest is required. There is no need to stay in hospital. The patient can resume his/ her activities in a couple of hours. It s entirely safe procedure. Usually a single sitting is sufficient. Few people with extensive lesions may require more than one sitting.
13. Does laser barrage give life long protection? Is there a need for yearly screening after laser barrage? Laser barrage does not prevent formation of holes in other areas. Consider a torn cloth. You stitch it. Does this prevent it in getting torn in other sites? Similarly, laser barrage treats only the existing lesions. Patient still has chance of developing lesions in other sites. Yearly screening and repeat laser, if required, are very much essential.
14. I underwent LASIK. Should I still undergo retinal screening?
Yes. LASIK only removes your glasses. It has no effect on your retinal status. Your thin retina still remains risky. LASIK does not reduce the chance of retinal breaks or RD.
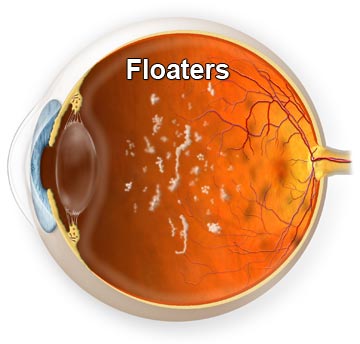
15. I am a myope. I sometimes see few black spots and strings infront of my eyes, especially when i look at sky. What are these?
These are called as “Floaters”. Myopia is a complex disorder with various problems. Glasses is just one of them. Myope have retinal problems. They may also have Vitreous Gel problems. Our eye ball is filled with a Vitreous gel. This gel is usually clear. In some myopes and even in normal people, this gel may get condensed in certain areas , forming opacities. These condensed vitreous strands are seen as spots or strings. These are innocuous and dangerless. But in few cases these floaters may be associated with retinal breaks. So you should undergo retinal screening to detect holes. If no holes are found, then you have nothing to worry. Sometimes you may see Flashes of light, which is called as photopsia. This is again an indication for immediate retinal screening, as it can be associated with retinal breaks.
16. What are the risk factors for Retinal detachment?
Myopia is the major risk factor.
Other risk factors are:
a. Previous cataract surgery.
b. Severe Injury.
c. Previous RD in other eye.
d. Family history of RD.
e. Retinal degenerations (which can be detected only by a retina surgeon) etc.
17. What is the treatment of Retinal Detachment?
There is no guaranteed treatment for RD. But there are treatments (Complex Vitreoretinal surgeries) which are aimed at reattaching the retina. But these should be considered as “Damage control measures” rather than guaranteed surgeries. Its like damage control done after a bomb explosion. Our aim should be to prevent the bomb explosion rather than doing damage control after explosion.
The available treatment modalities for RD are Scleral Buckling and Vitrectomy.
The type of surgery, type of anesthesia etc are decided by the characteristics of Retinal Detachment.
Scleral Buckle: A flexible band (Scleral buckle) is placed around the eye to counteract the force pulling the retina out of place.The fluid under the retina is drained off if necessary. This is an extraocularoperation with relatively less complications than vitrectomy.
Vitrectomy : This is intraocular procedure, where the surgical instruments enter the eyeball. The vitreous is removed, the subretinal fluid is removed and vitreous is replaced with air , fluid or silicon oil.
18. What are the risks of retinal surgery?
No surgery is riskless. RD surgery has some risks like Bleeding, Infection, Raised Intraocular pressure, Cataract etc..
The retina cannot be reattached even with all efforts in some cases
Most RD surgeries are successful, although a second operation is sometimes needed.
19. What are the visual expectations after surgery?
Vision may take many months to improve and in some cases may never return fully. The amount of visual recovery cannot be predicted before surgery. Its only a matter of luck and chance. Unfortunately some patients do not recover any vision.
20. What happens to the eye if RD surgery is not done?
It will slowly lose all existing vision and becomes totally blind. The eye will eventually become small and shrunken causing an ugly cosmetic appearance.
Retinal Detachment blindness has no cure.
Prevention is the only way.
Regular retinal screening and Timely LASER Barrage is the only way to prevent Blindness.
 Graph 1
Graph 1 Graph 2
Graph 2